Eugenio P. Mende DVM MSc
Keeping animals healthy is a top priority for farmers and veterinarians, and antibiotics, especially in the Philippine system of farming are essentially used to fight disease in animals. Proper and legal use of antibiotics in animals also means a safe and wholesome food supply and reduces the chance of bacterial transmission from animals to humans. This link between animal health and human health is captured by the term “One Health,” meaning animal health affects people and human health affects animals.
However, human and animal health experts agree that antibiotic resistance is currently a public health concern, which is why animal production practices include judicious use guidelines to ensure that antibiotics can be used to keep food animals healthy while minimizing the chance of resistant bacteria impacting human health. Farmers, veterinarians and PVDA-member companies that make medicines for animals have collaborated with the industry to develop and implement guidelines that maximize animal health and well-being while providing consumers with the safest food possible.
The US FDA is implementing a new policy beginning January 1, 2017, that will stop the use of medically important antibiotics to promote growth in farm animals. It is imperative that animals will only be given medically important antibiotics when they are necessary to treat, control and prevent diseases. When animals are given medically important antibiotics in feed or water, it will be under the oversight of a licensed veterinarian.
The call for prudent and proper use of antibiotic is not to ban its use. The cause of possible antibiotic residue and resistant, as I will be presenting here, is its misuse in the farm systems. In this issue, I am sharing with you some insights adapted from the US Food and Drug Administration’s new policy – that hopefully will help us evaluate the way we use antibiotics in keeping our food animals healthy.
Medicine and Antibiotic Use in Farms
Keeping animals healthy is a top priority for farmers and veterinarians; healthy animals mean a safe and wholesome food supply and in turn, healthy people. Veterinarians and farmers work together to create flock and herd health management programs to prevent diseases before they develop and spread. These programs are tailored to individual farms and their livestock and poultry, taking into account how and when to vaccinate for species-specific diseases and how to administer parasite controls. To prevent and manage infectious diseases, it is sometimes necessary for veterinarians and farmers to turn to antibiotics. Research has shown the proper use of antibiotics can keep food animals healthy and reduce the potential for harmful bacterial contamination of finished meat products.
Animal production practices include guidelines to ensure that animal antibiotics are used in a manner that minimizes the development of antibiotic resistance in human health. Under new US FDA guidance, medically important antibiotics will be labeled for use in food animals only to treat, control and prevent disease and illness and will be used exclusively under the supervision and prescription of a licensed veterinarian.
Benefits of Antibiotics:

Historically, some US FDA-approved antibiotics had been used to promote growth and weight gain in certain farm and flock animals. Antibiotics approved by the FDA are used to fight diseases in animals, which supports animal welfare and food safety for consumers.
Benefit to Animal Welfare
Ensuring animal welfare is a human responsibility; it includes proper housing, management, nutrition, disease prevention and treatment, responsible care and humane handling. Medicines, including antibiotics, are an important tool for veterinarians tasked with protecting animal health and preventing suffering from disease, which can lead to poor animal welfare.
Benefit to Food Safety
The benefits of using antibiotics to treat and prevent animal disease extend far beyond the farm. In fact, research has shown that as rates of animal illnesses increase, so do rates of human illness (Russell 2003, Hurd et al PHR 2008). At least one study has shown that even a slight increase in animal-illness rate leads to a greater human-illness rate than the development of antibiotic resistance.
Food safety begins with healthy animals, continues in meat processing with application of hygienic standards and pathogen reduction technologies, and extends to the handling of the food product in both the market and the home. All of these steps work in tandem as layers of protection to decrease the risk of food borne illness. Studies have shown that animals that are sub-clinically ill – not outwardly showing signs of illness – can increase bacterial contamination during meat processing. Use of antibiotics to prevent and control these low level infections is important in helping to reduce this type of contamination.
Risk of Antibiotics
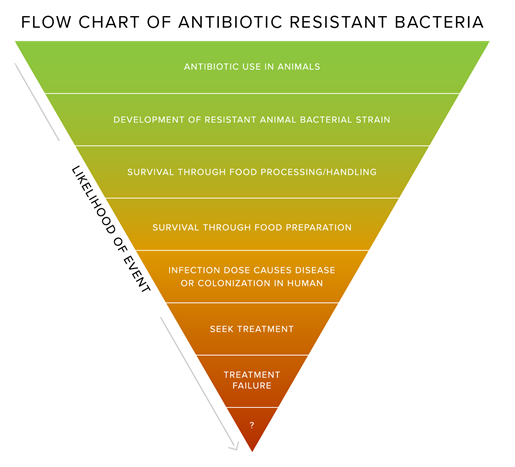
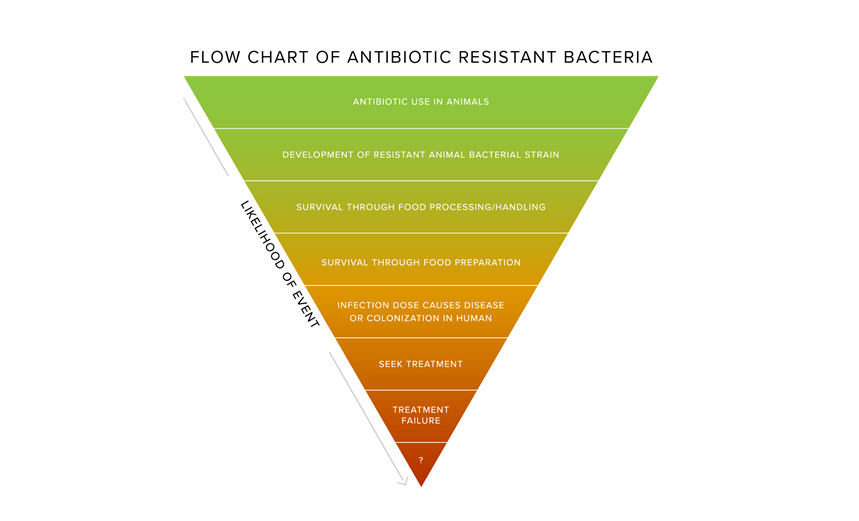
While it is possible that antibiotic resistant bacteria can transfer from animals to humans, the chances are extremely small that a person would contract an illness that cannot be treated with an antibiotic as a result of that person consuming food from animals treated with that antibiotic.
This is because in order for a person to contract an illness that could not be treated with an antibiotic, EACH of the events described in this chart would have to occur – and there are programs and interventions designed to kill or eliminate bacteria at many of those steps. Throughout food production and processing systems, there are strict standards that act as safeguards to human health in that they greatly reduce the presence of all bacteria, whether resistant or not. Furthermore, government data from monitoring of food borne bacteria in meat and poultry indicates that the prevalence of resistance is very low with those antibiotics of critical importance in human medicine.
The US FDA, animal medicine companies, and academic researchers have conducted several quantitative risk assessments on animal antibiotics, and these studies have consistently found very low risk to human health. These results demonstrate that the interventions used to keep bacteria from transferring from animals to humans are effective. They have also shown that not using antibiotics to fight diseases in animals could result in an increase in food borne illness.
To put into perspective the risk of experiencing antibiotic resistance due to consuming food that contains antibiotics, the Harvard Center for Risk Analysis calculated the following to compare the risk of acquiring a resistant bacterial infection compared to other risks:

Very timely shout out to look closely into antibiotic use.
Thanks Dr Eugene!